Breast Augmentation
- Home
- Breast Augmentation
 |
|
Breast augmentation is usually done to balance a difference in breast size, to improve body contour, or as a reconstructive technique following surgery.
|
Breast augmentation, technically known as augmentation mammoplasty, is a surgical procedure to enhance the size and shape of a woman’s breast for a number of reasons:
-
- To enhance the body contour of a woman who, for personal reasons, feels her breast size is too small.
- To correct a reduction in breast volume after pregnancy.
- To balance a difference in breast size.
- As a reconstructive technique following breast surgery.
By inserting an implant behind each breast, surgeons are able to increase a woman’s bustline by one or more bra cup sizes. If you’re considering breast augmentation, the following information will give you a basic understanding of the procedure – when it can help, how it’s performed, and what results you can expect. It can’t answer all of your questions, since a lot depends on your individual circumstances. Please ask your surgeon if there is anything you don’t understand about the procedure.
The best candidates for breast augmentation
Breast augmentation can enhance your appearance and your self-confidence, but it won’t necessarily change your looks to match your ideal, or cause other people to treat you differently. Before you decide to have surgery, think carefully about your expectations and discuss them with your surgeon.
The best candidates for breast augmentation are women who are looking for improvement, not perfection, in the way they look. If you’re physically healthy and realistic in your expectations, you may be a good candidate.
Types of implants
|
|
|
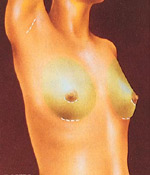
Incisions are made to keep scars as inconspicuous as possible, in the breast crease, around the nipple, or in the armpit. Breast tissue and skin is lifted to create a pocket for each implant.
|
A breast implant is a silicone shell filled with either silicone gel or a salt-water solution known as saline.
Because of concerns that there is insufficient information demonstrating the safety of silicone gel-filled breast implants, the Food & Drug Administration has determined that new gel-filled implants, at the present time, should be available only to women participating in approved studies. Some women requiring replacement of the implants may also be eligible to participate in the study.
Saline-filled implants continue to be available to breast augmentation patients on an unrestricted basis, pending further FDA review. You should ask your doctor more about the specifics of the FDA decisions. (Above guidelines are current as of July 1992.)
All surgery carries some uncertainty and risk
|
|
|
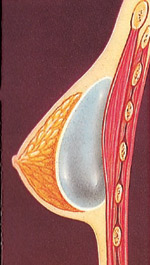
The breast implant may be inserted directly under breast tissue or beneath the chest wall muscle.
|
Breast augmentation is relatively straightforward. But as with any operation, there are risks associated with surgery and specific complications associated with this procedure.
The most common problem, capsular contracture, occurs if the scar or capsule around the implant begins to tighten. This squeezing of the soft implant can cause the breast to feel hard. Capsular contracture can be treated in several ways, and sometimes requires either removal or “scoring” of the scar tissue, or perhaps removal or replacement of the implant.
As with any surgical procedure, excessive bleeding following the operation may cause some swelling and pain. If excessive bleeding continues, another operation may be needed to control the bleeding and remove the accumulated blood.
A small percentage of women develop an infection around an implant. This may occur at any time, but is most often seen within a week after surgery. In some cases, the implant may need to be removed for several months until the infection clears. A new implant can then be inserted. Some women report that their nipples become oversensitive, undersensitive, or even numb. You may also notice small patches of numbness near your incisions. These symptoms usually disappear with time, but may be permanent in some patients.
There is no evidence that breast implants will affect fertility, pregnancy, or your ability to nurse. If, however, you have nursed a baby within the year before augmentation, you may produce milk for a few days after surgery. This may cause some discomfort, but can be treated with medication prescribed by your doctor.
|
|
|
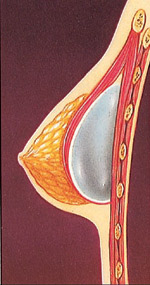
The breast implant may be inserted directly under breast tissue or beneath the chest wall muscle.
|
Occasionally, breast implants may break or leak. Rupture can occur as a result of injury or even from the normal compression and movement of your breast and implant, causing the man-made shell to leak. If a saline filled implant breaks, the implant will deflate in a few hours and the salt water will be harmlessly absorbed by the body.
If a break occurs in a gel-filled implant, however, one of two things may occur. If the shell breaks but the scar capsule around the implant does not, you may not detect any change. If the scar also breaks or tears, especially following extreme pressure, silicone gel may move into surrounding tissue. The gel may collect in the breast and cause a new scar to form around it, or it may migrate to another area of the body. There may be a change in the shape or firmness of the breast. Both types of breaks may require a second operation and replacement of the leaking implant. In some cases, it may not be possible to remove all silicone gel in the breast tissue if rupture should occur.
 |
|
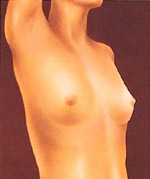
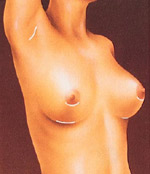
After surgery, breasts appear fuller and more natural in tone and contour. Scars will fade with time.
|
A few women with breast implants have reported symptoms similar to diseases of the immune system, such as scleroderma and other arthritis-like conditions. These symptoms may include joint pain or swelling, fever, fatigue, or breast pain. Research has found no clear link between silicone breast implants and the symptoms of what doctors refer to as “connective-tissue disorders,” but the FDA has requested further study.
While there is no evidence that breast implants cause breast cancer, they may change the way mammography is done to detect cancer. When you request a routine mammogram, be sure to go to a radiology center where technicians are experienced in the special techniques required to get a reliable x-ray of a breast with an implant. Additional views will be required. Ultrasound examinations may be of benefit in some women with implants to detect breast lumps or to evaluate the implant.
While the majority of women do not experience these complications, you should discuss each of them with your physician to make sure you understand the risks and consequences of breast augmentation.
Planning your surgery
In your initial consultation, your surgeon will evaluate your health and explain which surgical techniques are most appropriate for you, based on the condition of your breasts and skin tone. If your breasts are sagging, your doctor may also recommend a breast lift. (For more in formation on this procedure, ask your physician for the ASPRS brochure on breast lift, also known as mastopexy.)
Be sure to discuss your expectations frankly with your surgeon. He or she should be equally frank with you, describing your alternatives and the risks and limitations of each. You may want to ask your surgeon for a copy of the manufacturer’s insert that comes with the implant he or she will use-just so you are fully informed about it. And, be sure to tell your surgeon if you smoke, and if you’re taking any medications, vitamins, or other drugs.
Your surgeon should also explain the type of anesthesia to be used, the type of facility where the surgery will be performed, and the costs involved. Because most insurance companies do not consider breast augmentation to be medically necessary, carriers generally do not cover the cost of this procedure.
Preparing for your surgery
Your surgeon will give you instructions to prepare for surgery, including guidelines on eating and drinking, smoking, and taking or avoiding certain vitamins and medications.
While making preparations, be sure to arrange for someone to drive you home after your surgery and to help you out for a few days, if needed.
Where your surgery will be performed
Your surgeon may prefer to perform the operation in an office facility, a freestanding surgery center, or a hospital outpatient facility. Occasionally, the surgery may be done as an inpatient in a hospital, in which case you can plan on staying for a day or two.
Types of anesthesia
Breast augmentation can be performed with a general anesthesia, so you’ll sleep through the entire operation. Some surgeons may use a local anesthesia, combined with a sedative to make you drowsy, so you’ll be relaxed but awake, and may feel some discomfort.
The surgery
The method of inserting and positioning your implant will depend on your anatomy and your surgeon’s recommendation. The incision can be made either in the crease where the breast meets the chest, around the areola (the dark skin surrounding the nipple), or in the armpit. Every effort will be made to assure that the incision is placed so resulting scars will be as inconspicuous as possible.
Working through the incision, the surgeon will lift your breast tissue and skin to create a pocket, either directly behind the breast tissue or underneath your chest wall muscle (the pectoral muscle). The implants are then centered beneath your nipples.
Some surgeons believe that putting the implants behind your chest muscle may reduce the potential for capsular contracture. Drainage tubes may be used for several days following the surgery. This placement may also interfere less with breast examination by mammogram than if the implant is placed directly behind the breast tissue. Placement behind the muscle however, may be more painful for a few days after surgery than placement directly under the breast tissue.
You’ll want to discuss the pros and cons of these alternatives with your doctor before surgery to make sure you fully understand the implications of the procedure he or she recommends for you. The surgery usually takes one to two hours to complete. Stitches are used to close the incisions, which may also be taped for greater support. A gauze bandage may be applied over your breasts to help with healing.
After your surgery
You’re likely to feel tired and sore for a few days following your surgery, but you’ll be up and around in 24 to 48 hours. Most of your discomfort can be controlled by medication prescribed by your doctor.
Within several days, the gauze dressings, if you have them, will be removed, and you may be given a surgical bra. You should wear it as directed by your surgeon. You may also experience a burning sensation in your nipples for about two weeks, but this will subside as bruising fades.
Your stitches will dissolve over time, but the swelling in your breasts may take three to five weeks to disappear.
Getting back to normal
You should be able to return to work within a few days, depending on the level of activity required for your job.
Follow your surgeon’s advice on when to begin exercises and normal activities. Your breasts will probably be sensitive to direct stimulation for two to three weeks, so you should avoid much physical contact. After that, breast contact is fine once your breasts are no longer sore, usually three to four weeks after surgery.
Your scars will be firm and pink for at least six weeks. Then they may remain the same size for several months, or even appear to widen. After several months, your scars will begin to fade, although they will never disappear completely.
Routine mammograms should be continued after breast augmentation for women who are in the appropriate age group, although the mammographic technician should use a special technique to assure that you get a reliable reading, as discussed earlier.
Your new look
For many women, the result of breast augmentation can be satisfying, even exhilarating, as they learn to appreciate their fuller appearance.
Regular examination by your plastic surgeon and routine mammograms for those in the appropriate age groups at prescribed intervals will help assure that any complications, if they occur, can be detected early and treated.
Your decision to have breast augmentation is a highly personal one that not everyone will understand. The important thing is how you feel about it. If you’ve met your goals, then your surgery is a success.